Managing the pathogenic pathways by which disease develops and progresses provides one of the most effective ways to manage rheumatologic disease. Etanercept transformed the treatment of RA by blocking TNF, but even more targeted agents might be more effective with greater safety. That’s the thought behind the Accelerating Medicines Partnership program to unravel the molecular action of rheumatoid arthritis at the cellular level.
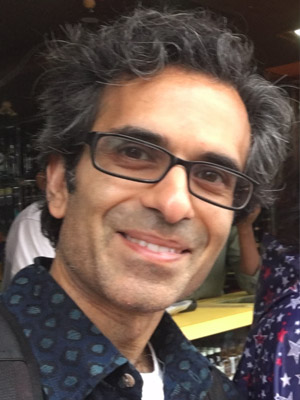
“Tissue inflammation is central to many human diseases, including rheumatic diseases. Investigators have been trying to understand it for a long time,” said Soumya Raychaudhuri, MD, PhD, Professor of Medicine at Harvard Medical School and Director of the Center for Data Sciences at Brigham and Women’s Hospital. “What is different now is that we are looking at individual genes in single cells from inflamed joints of patients with RA, and in the process finding novel details about molecular pathways that will help us better personalize care.”
Dr. Raychaudhuri will explore some of the latest findings in RA during the Accelerating Medicines Partnership (AMP): Molecular Deconstruction of RA Symposium on Monday from 1:00 – 2:00 pm in Hall B1, Building B in the Georgia World Congress Center. Early findings are already changing perspectives on RA research and treatment.
Phase I, data collection, has already started to highlight differences and abnormalities in immune and tissue cell populations with single-cell gene expression data. Phase II will obtain single-cell gene expression data on thousands of cells from more than 100 RA patients. Sample collection is largely complete; sample processing and data analysis are ongoing.
The goal is to identify novel pathways that might be exploited for diagnostic, prognostic, and herapeutic use.
Interleukin-6 (IL-6), for example, has been recognized as an effective target. The first anti-IL-6 agent, tocilizumab, was approved by the FDA in 2017. It was clear from research and clinical trial data that the agent can be highly effective against RA, but the precise cell-types that produced IL-6 within the inflamed joint were less clear. New details are emerging.
“We are just starting to look at the data we have gathered so far and are already seeing things that had not been apparent before,” Dr. Raychaudhuri said. “One of the big surprises has been that IL-6 is secreted from a very specific subset of fibroblasts. There are going to be a lot more such surprises along the way.”
Single-cell RNA analysis shows which genes are turned on and turned off within specific cells, he said. Gene expression is clearly different for different cell populations in different tissues affected by RA. What is more surprising, and potentially more clinically useful, is seeing how gene expression changes in the same cell populations as the cells change in response to specific environmental factors.
Tracking the activity of thousands of genes in each of thousands of cells generates enormous data sets, Dr. Raychaudhuri noted. And the data are far from perfect.
“What I spend most of my time and energy and life doing is trying to understand these data sets, trying to interpret them, trying to develop algorithms that can help us understand what is going on in these different types of cells,” he said.
“One of the key goals is to understand how the differences in cellular content and cellular states contribute to a given patient endpoint. We want to be able to predict, from looking at a patient’s own cells, which drugs they are going to respond to, whether they are likely to go into remission or whether they are likely to have a more severe course and need more aggressive treatment. This kind of data will enable us to deliver on the promise of precision medicine.”
