Showcasing cutting-edge rheumatology research from around the world, six of the top abstracts submitted for this year’s Annual Meeting were presented during Tuesday’s Plenary III session.
Mitochondrial Contribution to Juvenile Dermatomyositis Pathogenesis

Researchers report that novel findings of mitochondrial antibodies in juvenile dermatomyositis (JDM), preceding clinical diagnosis of calcinosis, support mitochondrial extrusion as a potential therapeutic targetable pathway, and the use of anti-mitochondrial antibodies (AMAs) as prognostic markers, allowing for early, preventive treatment, reducing development of disabling calcinosis in those children.
“Using electron microscopy of untreated patients, we visualized the mitochondria in JDM muscle tissue and found, to our surprise, that the mitochondria were crystallized, unable to function properly, and therefore not able to support the muscle with sufficient energy,” said Christian Lood, PhD, Assistant Professor in the Division of Rheumatology at the University of Washington in Seattle. “Further, we found evidence of extracellular mitochondria, with mitochondrial protein and DNA in peripheral circulation, in particular in patients with ongoing muscle disease activity as well as calcinosis.”
Dr. Lood also reported that they found a novel autoantibody targeting mitochondria able to predict development of severe disabling calcinosis.
“This is clinically significant and may allow identification of children at risk of calcinosis early enough to initiate preventive treatment,” he said. “Our study thus implicates an important role of mitochondria in JDM pathogenesis and suggests that preventing mitochondrial damage may be a novel therapeutic target in JDM.”
Efficacy and Safety of Upadacitinib in a Randomized, Double-Blind, Placebo-Controlled, Multicenter Phase 2/3 Clinical Study of Patients with Active Ankylosing Spondylitis

In this study, researchers report that upadacitinib (15mg QD) was significantly more efficacious than placebo in patients with active ankylosing spondylitis (AS) for improvement in signs and symptoms, function, and imaging. The proportion of patients with adverse events was similar in the upadacitinib and placebo arms, and no new safety findings were observed compared with previous upadacitinib studies in other diseases.
“The study met its primary endpoint of ASAS40 response at week 14 and several multiplicity-controlled secondary endpoints related to signs and symptoms of AS, function, and MRI detected active inflammation at week 14,” said Désirée van der Heijde, MD, PhD, Professor of Rheumatology at Leiden University Medical Center, Netherlands.
Regarding safety, Dr. van der Heijde said that no serious infections, herpes zoster, tuberculosis, malignancies, gastrointestinal perforations, renal dysfunction, anemia, lymphopenia, adjudicated major adverse cardiovascular events, venous thromboembolic events, or deaths were reported.
“These results support further investigation of upadacitinib for the treatment of axial spondyloarthritis,” she said.
Ixekizumab in Non-Radiographic Axial Spondyloarthritis: Primary Results from a Phase 3 Trial

Ixekizumab significantly improved the signs and symptoms of non-radiographic axial spondyloarthritis (nr-axSpA) after 52 weeks as measured by ASAS40 in patients with objective signs of inflammation who are bDMARD-naïve at 16 and 52 weeks, the primary endpoint of the study. Ixekizumab also met the major secondary endpoints in the study at week 16 and week 52.
“In this study, a total of 303 adult patients with active nr-axSpA were randomized to receive ixekizumab 80 mg subcutaneously every four weeks or every two weeks, following 80 mg or 160 mg starting dose at week 0, or placebo,” said Atul Deodhar, MD, MRCP, Professor of Medicine and Medical Director of the Rheumatology Clinic for the Division of Arthritis and Rheumatic Diseases at Oregon Health & Science University in Portland.
“The positive results provide evidence that ixekizumab could become the first IL-17A antagonist to be approved in the U.S. for people with this chronic, debilitating inflammatory disease,” Dr. Deodhar said. “This is significant, as there are currently limited biologic treatment options beyond TNF-inhibitors available for affected patients.”
Efficacy and Safety of Romosozumab vs. Placebo Among Patients with Mild-to-Moderate Chronic Kidney Disease

In this post hoc analysis of the FRAME study, investigators found that romosozumab increased bone mineral density (BMD) across eGFR subgroups versus placebo, and the reduction in new vertebral fractures was not notably affected by eGFR level. Safety was also generally comparable among eGFR subgroups, according to Jonathan Adachi, MD, FRCP, Professor of Medicine at the Michael DeGroote School of Medicine at McMaster University and Director of the Hamilton Arthritis Centre at St. Joseph’s Healthcare in Hamilton, Ontario, Canada.
FRAME was a randomized Phase 3 clinical trial that enrolled 7,180 postmenopausal women with T-scores –2.5 to –3.5 at the total hip or femoral neck. In the placebo-controlled double-blind period, patients received romosozumab 210mg or placebo monthly for 12 months.
“Based on our findings, romosozumab could be considered as a treatment option for osteoporotic patients with mild-to-moderate CKD,” Dr. Adachi said. “To further assess the efficacy and safety of romosozumab in patients with different levels of renal function, we are looking into the second pivotal trial, the ARCH study, which enrolled a population at a higher fracture risk compared with FRAME.”
Decomposition Analysis of Spending and Price Trends for Biologic Anti-Rheumatic Drugs in Medicare and Medicaid
Researchers found that annual spending on biologic DMARDs by U.S. public programs and beneficiaries nearly doubled from 2012 to 2016. The study showed post-market drug price changes alone account for the majority of recent spending growth, and manufacturers’ rebates have little impact on rising costs.
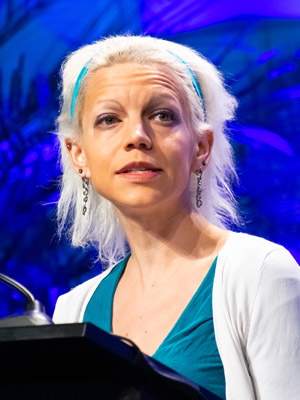
“We accessed drug spending data from the Centers for Medicare and Medicaid Services (CMS) for years 2012 through 2016. It contained spending and utilization data from prescription medication claims processed across the Medicare Part D, Medicare Part B fee-for-service, and Medicaid programs, thus covering more than 41 million beneficiaries in 2016,” said Natalie McCormick, PhD, MSc, a post-doctoral fellow at Massachusetts General Hospital and Harvard Medical School. “All biologic DMARDs with FDA approval for at least one rheumatic disease through December 2014 were eligible for inclusion; that cut-off was chosen to allow us to assess trends over at least two years.”
While proposals to remove rebates or pass them along to consumers may help some beneficiaries, Dr. McCormick said that more changes are needed to control public spending and patients’ out-of-pocket costs for these potent treatments.
“In the meantime, with prices continuing to rise, our findings underlie the importance of rheumatologists and patients discussing the costs of biologic DMARD treatment and options for mitigating cost concerns and barriers to effective treatment,” she said.
The Relationship Between Gout and Cardiovascular Disease Outcomes: A Health Data Linkage Study of 1 Million New Zealanders Using Population-level Cardiovascular Risk Prediction Equations

Findings from this study suggest that gout is associated with an increased estimated risk of cardiovascular disease (CVD) events calculated from population-level cardiovascular risk equations. Even after adjustment for estimated five-year CVD risk and additional weighting of risk factors within it, gout independently increased the odds for fatal and non-fatal events, an effect that was not ameliorated by allopurinol use or serum urate lowering to treatment target, according to Ken Cai, MBBS, MSc(Med), Rheumatology Clinical Fellow at the University of Auckland in New Zealand.
“Compared with people without gout, there was no statistically significant difference in adjusted hazard ratio for CVD among those with gout who were dispensed allopurinol compared with those not dispensed allopurinol,” Dr. Cai said.
There was also no statistically significant difference in adjusted hazard ratio for those with serum urate above 6mg/dL or below 6mg/dL, he said, when compared to people without gout.
“Our study adds to the growing body of evidence to support the importance of evaluating CVD risk in people with gout,” Dr. Cai said.
