Osteoporosis has led to an increasing public health risk as more people, both women and men, suffer from osteoporotic fractures as they age. While reliable methods for screening and treatment exist, questions and dilemmas remain. Three experts in the science and treatment of osteoporosis discussed current controversies in managing the disease day to day.
The session, Controversies and Updates in Osteoporosis Management, is available on demand for registered ACR Convergence 2023 participants through Oct. 31, 2024, on the meeting website.
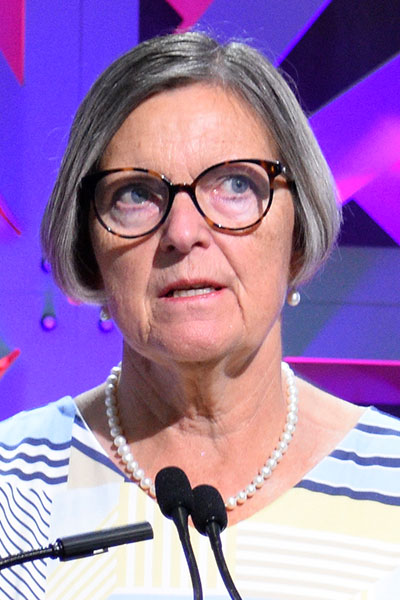
Bente Langdahl, MD, PhD, Professor at Aarhus University and Consultant at the Department of Endocrinology and Internal Medicine at Aarhus University Hospital, Denmark, addressed the use of denosumab, and how and what to transition to after its use. The novel agent has been shown to reduce bone turnover, improve bone mineral density, and reduce fracture risk, according to the National Institutes of Health.
Patients who received denosumab showed long-term increases in bone mineral density (BMD) in the hip and spine compared with other treatments, such as bisphosphonates.
“In placebo-treated patients enrolled in the FREEDOM trial, compared with patients treated with denosumab, over 10 years you can see a robust reduction in all types of fractures for patients on denosumab,” Dr. Langdahl said.
But this benefit is reversible, and in some cases rapidly reversible, she said. Post-hoc analysis of the FREEDOM trial showed an increased risk of multiple fractures after discontinuing use of denosumab. Research has shown a gradual decrease in the amount of denosumab can result in less rapid BMD loss.
Ultimately, there is an expectation of bone loss in patients on long-term denosumab treatment, she said; however, it may be worthwhile to aim for higher BMD before considering stopping the drug.

Richard Eastell, BSc (Hons), MBChB, MD (Edin), FRCP (London, Edin), FRCPI (Hon), FRCPath, FMedSci, Professor of Bone Metabolism and Director of the Mellanby Centre for Musculoskeletal Research at the University of Sheffield, United Kingdom, made the case that bone turnover markers (BTMs) are ready for more widespread use in managing osteoporosis.
BTMs reflect the activity of bone cells, Dr. Eastell said, and C-telopeptide of type I collagen (CTX) and N-telopeptide of type I collagen (NTX) have been recognized internationally as reference markers.
The TRIO study showed that CTX and serum procollagen type I N-propeptide (PINP) were reliable BTMs. They resulted in the highest percentage of change from baseline in patients being treated with alendronate from 12 to 24 weeks.
With BMD measurements, changes can be small and slow, and elderly patients can produce unreliable results, Dr. Eastell said. But with BTMs, changes are significant and occur early. The International Osteoporosis Foundation (IOF) and the European Calcified Tissue Society (ECTS) have developed working groups that support BTMs.
The general practice population has embraced BTMs because they are relatively cost effective and provide more convenient monitoring for patients.
“What we’ve found was the use of BTMs has improved clinical outcomes,” Dr. Eastell said. “In the USA, the use of BTMs does seem to be helping in decision-making, and the uptake has been slow but is on the rise.”

Connie Weaver, PhD, MS, Distinguished Research Professor in Exercise and Nutritional Sciences at San Diego State University, Distinguished Professor Emerita of Nutrition Science at Purdue University, and CEO of Weaver and Associates Consulting, LLC, provided an update on vitamin D supplementation and monitoring. There is a prevalence of deficiency of vitamin D in many areas of the world.
Vitamin D influences bone through muscles and intestines, and a meta-analysis shows calcium plus vitamin D reduces the risk of hip fractures by 30%. The main sources of vitamin D are in fortified milk and supplements, and both D2 and D3 are biologically active.
VITAL, a study of more than 25,000 patients over five years, challenged the current recommendations for vitamin D, which are all based on bone health parameters.
“The study looked at cumulative fracture in various sites, and there’s nothing distinguishable between the placebo and the vitamin D3,” Dr. Weaver said. “Free vitamin D is more likely predictive of musculoskeletal health.”
Register Today for ACR Convergence 2025

If you haven’t registered for ACR Convergence 2025, register today to participate in this year’s premier rheumatology experience, October 24–29 in Chicago. All registered participants receive on-demand access to scientific sessions after the meeting through October 31, 2026.
