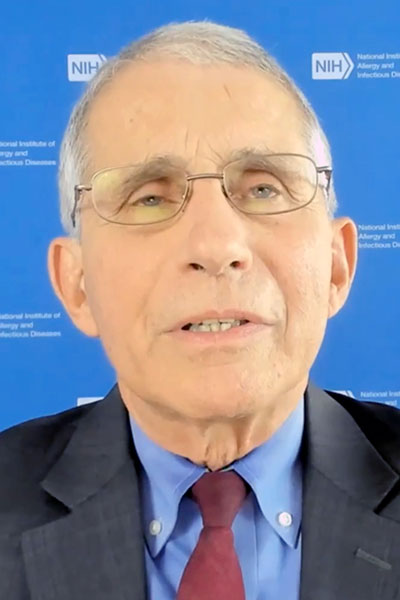
Before delivering his address during ACR Convergence 2020, Anthony S. Fauci, MD, was awarded the ACR Distinguished Global Public Health Award during the special session COVID-19: Public Health and Scientific Challenges.
“I started my NIH career studying rheumatologic disease,” Dr. Fauci said. “As an erstwhile rheumatologist, it is my special honor to be recognized by the ACR.”
Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a leading proponent of a coordinated, nationwide public health-focused response to the COVID-19 pandemic, is also an ACR Master and delivered the 2017 annual meeting keynote on vaccine development during epidemics. Registered ACR Convergence 2020 attendees have on-demand access to watch a replay of this year’s presentation through Wednesday, March 11.
COVID-19 is the worst pandemic since the influenza pandemic of 1918, he said, but it is not our first experience with coronaviruses. Four familiar coronaviruses are responsible for nearly a third of the annual common cold illnesses that strike as winter moves around the globe.
SARS was the first truly pandemic coronavirus when it emerged as a human pathogen in 2002 via bats and civet cats. It caused about 8,000 cases worldwide and some 800 deaths, Dr. Fauci noted, but was not particularly efficient in human to human spread.
“Public health measures, including quarantining and contract tracing, extinguished the outbreak without further intervention.”
MERS, which emerged from bats by way of camels in 2012, is still seen from time to time, but has largely disappeared from the global landscape.
COVID-19 is different. The U.S. case-fatality rate is 2.3%, less than SARS, but the virus is far more efficient in spreading from human to human. As of early November, nearly 50 million cases had been reported worldwide and 1.2 million deaths.
“The U.S. has been hit the worst of any country,” Dr. Fauci said.
Europe was hit at least as hard by an initial wave of infection early this year, he continued, but Spain, Italy and other hard-hit countries brought their infection rates down to a low baseline using familiar public health measures, quarantines, social distancing, and contract tracing.
Both the U.S. and the EU have seen a resurgence of cases, but the U.S. is faring far worse. U.S. infection rates never declined to the low levels seen in Europe because the U.S. lacked a unified public health response.
“We had a resurgence in June resulting from attempts to so-called reopen the economy,” Dr. Fauci said, which was done with different adherence to public health guidelines. “Different states did things differently. And when you look at GPS data, you clearly see that the U.S. never successfully reduced travel and interpersonal contact.”
The NIH recommends just two therapeutics for COVID-19, remdesivir, an investigational antiviral, and dexamethasone. Both are recommended only for specific hospitalized populations. Current guidelines are available at Covid19treatmentguidelines.nih.gov.
The U.S. is currently funding development of vaccine candidates across three platforms, Dr. Fauci continued.
Moderna and Bionetch/Pfizer are developing nucleic acid products. Oxford/AstraZeneca, Janssen/Johnson & Johnson, and Merck are developing viral vector products. Novax and GSK/Sanofi are developing protein subunit products.
Depending on phase 3 trial results, which could be released by late November, the first doses of vaccine, earmarked for healthcare and other frontline providers, could be available in early 2021.
The medical reality, Dr. Fauci said, is that control of COVID-19 depends more on public health measures that are available today than on therapeutics and vaccines that remain in the indefinite future. SARS-CoV-2 is transmitted primarily through respiratory droplets and aerosols that remain in the air over time and less commonly through contact with contaminated surfaces.
Broad implementation of five measures could dramatically reduce transmission and reduce the burden of COVID-19:
- Universal wearing of masks/cloth face coverings
- Maintaining at least six feet of physical distance
- Avoiding crowds and settings where people congregate
- Remaining outdoors rather than indoors
- Washing hands frequently
“If those five public health measures were adhered to universally and consistently over the country, it is clear that we would not be experiencing the surge of cases that we are currently seeing,” he said.
