This year’s Great Debate focused on the value of tapering biologic DMARDs (bDMARDs) in patients with rheumatoid arthritis who have achieved low disease activity (LDA).
Paul Emery, MD, MA, FRCP, Arthritis Research UK Professor of Rheumatology, Director of the Leeds Institute of Rheumatic and Musculoskeletal Medicine, and Director of the Leeds Musculoskeletal Biomedical Research Centre at Leeds Teaching Hospitals Trust, argued in favor of tapering. Arthur Kavanaugh, MD, Professor of Medicine and Director of the Center for Innovative Therapy, University of California, San Diego, took the opposite side during To Taper or Not to Taper? – Biologic DMARDs in Low Rheumatoid Arthritis Disease Activity.
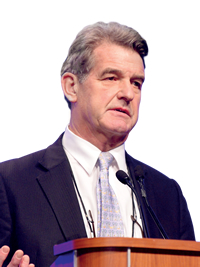
Dr. Emery said that tapering was not only highly desirable but extremely possible in early disease and also in established disease under certain circumstances. He said that the points he made during Sunday’s debate fell in line with EULAR recommendations established in 2013 and a 2016 update that reduction of TNF inhibitors (TNFi) after achieving and sustaining a disease activity score (DAS28) of less than 2.6 in early and established RA enables excellent outcomes.
Dr. Emery focused on tapering’s benefit when used in conjunction with early treatment. Clinicians are meant to get patients into remission within six months, and he recommended that treatment should start at presentation with the goal of getting them to remission in six months, which also offers the best chance of tapering. The developing data about early treatment and tapering could impact future disease management.
“You get the opportunity to de-bulk the disease and the opportunity then to forget about radiographic damage,” he said. “But I make the point that at the moment the only remission data we have is from treating very severe patients. I would say that we’ve gotten it all wrong. We should be treating really mild patients to the level that nearly everyone can taper and the majority can actually stop therapy.”
Tapering or stopping bDMARD treatment logically would provide a cost benefit, he said. For example, 12 months of therapy for 90 percent of patients would cost about a quarter of what it costs for 20 years of therapy for 20 percent or more of patients.
“So the unthinkable is that the first use of biologics could be cost-effective, and if the reason that we do it is that, I think that’s really good reason for tapering,” he said.
Among the studies he presented was the OPTIMA study of withdrawal of adalimumab in early RA patients. Six months after stopping, there was roughly a 10 percent loss of response.
As Dr. Emery sees it, of the 10 patients who achieved LDA with the combination, one will flare even if adalimumab is continued and eight will not flare if adalimumab is stopped. So adalimumab continuation makes a difference in only 10 percent, and data from other studies shows a recapture of response in 75 percent of cases. That means around three percent of patients will have problems.
“So you’re spending a lot of money for 3 percent complications,” he said.
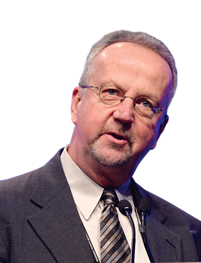
Dr. Kavanaugh said that while the data shows that some RA patients in LDA may have some prolonged clinical benefits after stopping TNFi, he sees the issue as whether the glass is half full or half empty. He cited the CORRONA registry involving LDA patients who decided to stop TNFi. While 73 percent went about two years without a flare and the midpoint was 18 months without a flare, almost everybody eventually flares.
“You can interpret this data in several ways,” he said. “The current theme, and one that’s going to have great importance to us practically, is that it’s really hard to know who’s going flare versus who’s going to have persistent benefit. It’s hard for us to pick that ahead of time.”
And those flares have consequences, Dr. Kavanaugh said. Patients incur damage with each flare, and damage leads to changes in functional status.
The BeSt study included TNFi tapering as part of the protocol. In that study, 8 percent of those patients never did well again after tapering.
“So the data say sure, you can try this, but 8 percent of your patients were doing fine. You changed their therapy around, and now they never get back to where they were. Is that good or not so good?” he asked.
Another concern for Dr. Kavanaugh is the inability right now to determine who’s a good candidate for tapering. There’s currently no proven way to predict with any accuracy who would do well with tapering despite some studies, such as HONOR, that have tried to connect the dots.
“That’s great for publications. It’s great for science, but it doesn’t help me in the clinic,” he said. “I need something that’s very, very predictive before I’m going to take Mrs. Jones and say let’s cut back on your treatment.”
Dr. Kavanaugh also has concerns about tapering’s impact on other manifestations of RA, including cardiovascular outcomes. Tapering, even though it would take inflammation a while to get going, potentially could increase the exposure to and risk of cardiovascular disease, for example.
The discussion isn’t just a medical or scientific discussion, Dr. Kavanaugh said. It’s an ethical issue that puts the medical community in a precarious spot if tapering is done for purely financial reasons — the “800-pound gorilla in the room,” he said —without knowing what the true benefit is.
Dr. Kavanaugh summed up his side with a Texas expression.
“Don’t poke a skunk. If you’re doing well, keep on treatment and keep doing well,” he said.
