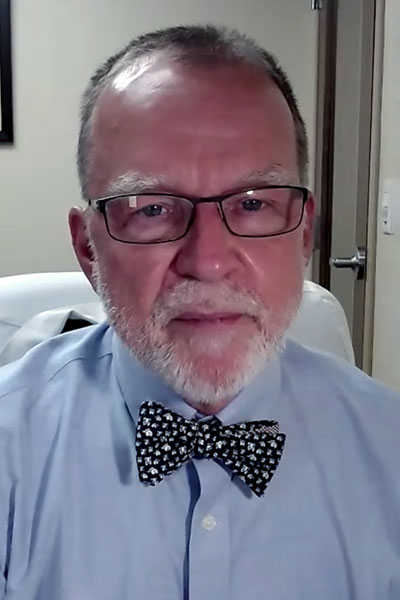
In 2012 and 2013, the Rheumatoid Arthritis Practice Performance (RAPP) project launched to address care gaps in RA disease control, which often center around how disease activity is measured, according to David Sikes, MD, Florida Medical Clinic.
During the session Optimize Clinical Teams to Increase Access to Care, Dr. Sikesreviewed how this project to re-engineer rheumatology practice was developed. Registered attendees have on-demand access to watch a replay of the session through Wednesday, March 11, 2021.
The initial concept of RAPP was to train rheumatology practices to measure disease activity at every visit, use that data to manage patients in a treat-to-target fashion, and collect data in a simple patient registry to manage the entire practice.
“You can then go back and look at how your patients are doing, how you’re doing, and when you see places that may not be as good, where you have a care gap, you can go back and address it,” Dr. Sikes said.
RAPP processes follow the philosophy that disease control needs to be the primary driver of transformation for a rheumatology practice, he said. Using the treat-to-target model, patients who have controlled or low disease activity should be assessed every six months. For patients with moderate or high disease activity, the recommended frequency for assessment increases to every three months.
However, data from 29,000 patients showed that 43% of patients with low disease activity were seen within the recommended timeframe. That number dropped to 27% for patients with high disease activity.
“The primary reason for the on-time assessment gap was a bottleneck—a classic business bottleneck—caused by too few visit slots, and this didn’t provide for on-time assessments,” Dr. Sikes said. “Essentially, the rheumatologist is the bottleneck. We’re the ones who have to see the patients. We do all the care.”
In response, the RAPP project identified several steps RA practices could take:
- Reducing the primary scope of patients seen to those with autoimmune inflammatory disease
- Reorganizing the practice to empower staff
- Tracking visit volumes and wait times, disease activity, and financial progress
Of the 170 RAPP-trained rheumatologists, 166 adopted the project processes to varying degrees. In those with the most complete adoption, including Dr. Sikes’ practice, noteworthy trends emerged.
“In all these practices, there were dramatic changes with simultaneous improvement in new patient waiting time, often going from six months and three months into the one-month period,” Dr. Sikes said.
Each of the practices also reported improvements in disease activity scores, patient satisfaction, and financial performance.
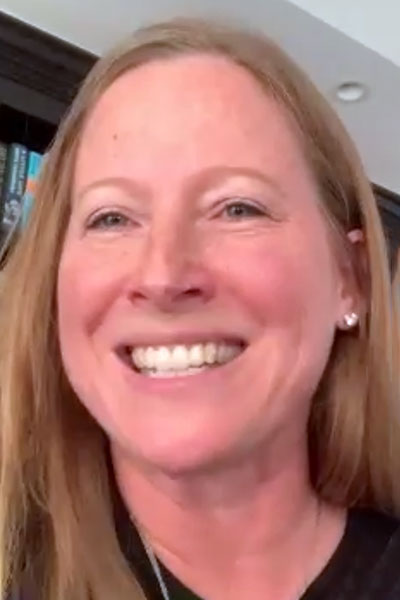
“We’re not just pushing larger numbers of patients through the door,” said Erin Arnold, MD, Orthopaedics and Rheumatology of the North Shore, Skokie, Illinois. “We’re actually doing a better job of taking care of them.”
Dr. Arnold is a partner at another practice with near complete adoption of RAPP processes. Her clinic was founded in order to implement the RAPP project.
In addition to clearly defining its patient population, Dr. Arnold’s practice outlined the responsibilities and expectations of the patient such as establishing a credit card on file. The practice also implemented a “meaningful” no-show fee and no longer reschedules new patients who do not show up for their first visit without canceling in advance.
The staff is organized with a team approach and clearly identified roles for each team member based on their training, leaving the physician to do “what only the physician can do”—synthesizing all of the information about individual patients to make management decisions, Dr. Arnold said.
From 2014 to 2019, her practice experienced a dramatic increase in the number of low RA disease activity patients and significant drops in the number of patients in the moderate and high disease activity groups. She attributes the changes to the separation of management and assessment visits.
“It makes a world of difference to have all of the information in front of you when you’re making decisions with the patient,” Dr. Arnold said.
Improved productivity, as well increased satisfaction among practice physicians and staff, have been among the unintended benefits of the switch to the treat-to-target approach. “Everybody has a role, and they all understand why they’re being asked to do that role if you take the time to train them,” Dr. Arnold said.
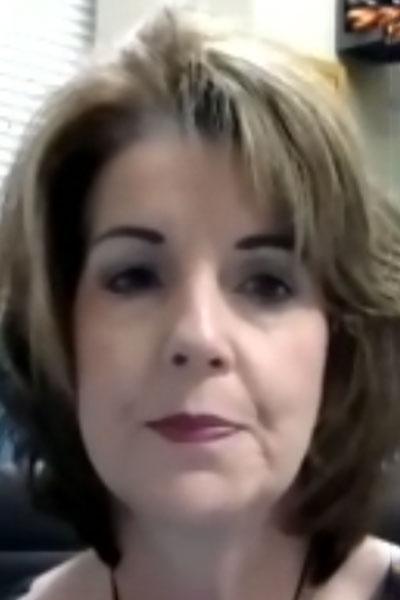
Treat-to-target also has shown to boost patient satisfaction, said Rosemary Walters, practice manager at Rheumatology Associates, PLLC, in Louisville, Kentucky. At the clinic where she works, productivity is up and there are more time slots for both new and existing patients in the schedule following the RAPP project.
